Mullerian anomalies are a group of congenital conditions that affect the development of the female reproductive system. These anomalies result from developmental issues during fetal growth, where the Mullerian ducts, which are responsible for forming the uterus, fallopian tubes, cervix, and upper two-thirds of the vagina, do not develop normally. The exact causes of Mullerian anomalies remain unclear, but they can have significant impacts on fertility, pregnancy, and sexual health. In this blog, we will explore what Mullerian anomalies are, their various types, and how they are diagnosed and treated.
What Are Mullerian Anomalies?
The Mullerian ducts begin forming during the early stages of fetal development and are the precursors to the female reproductive organs. Any disruption in this process can lead to Mullerian anomalies, which are categorized based on the severity and specific structures affected. These conditions can range from minor abnormalities to major malformations that impact fertility and reproductive health.
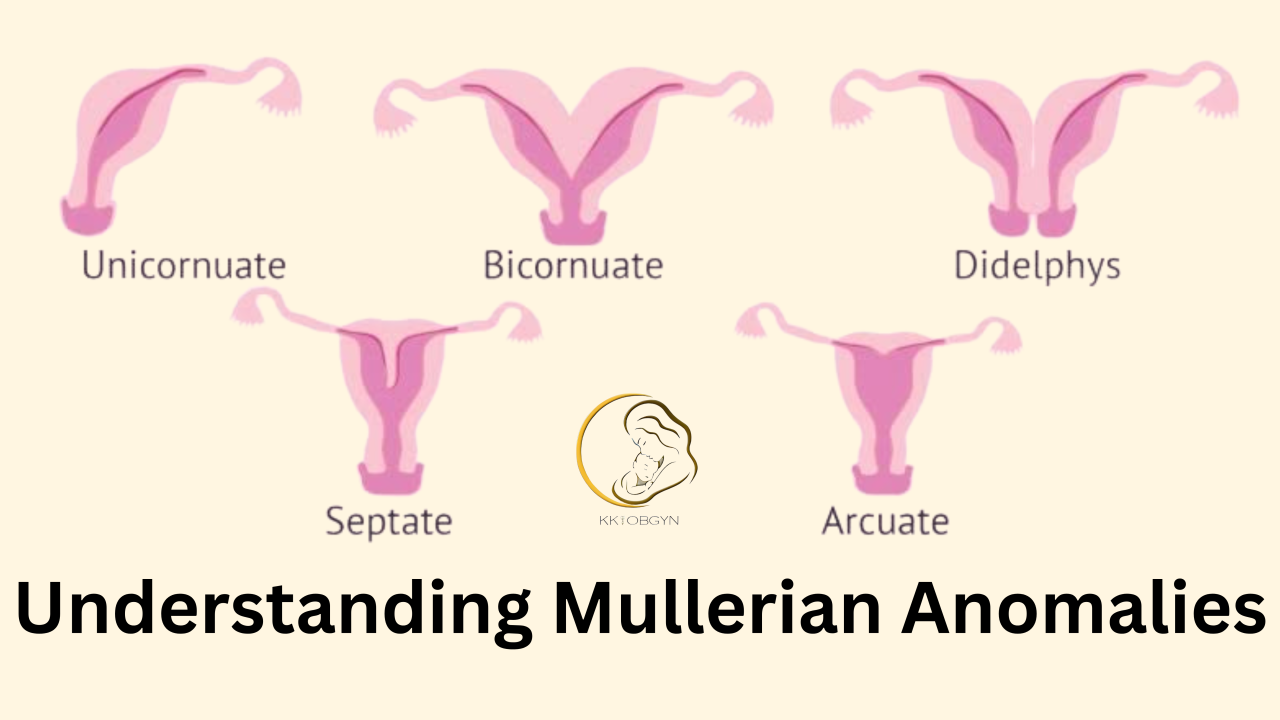
Types of Mullerian Anomalies
Mullerian anomalies are classified into several types, depending on the degree of abnormality. Here are the most common classifications:
1. Agenesis/Hypoplasia of the Mullerian Ducts
- Mayer-Rokitansky-Küster-Hauser Syndrome (MRKH): One of the most well-known forms of Mullerian agenesis, MRKH involves the congenital absence or underdevelopment of the uterus and the upper two-thirds of the vagina. Women with MRKH typically have normal ovarian function, so they may go through puberty and develop secondary sexual characteristics like breast development and pubic hair growth, but they will be unable to carry a pregnancy.
2. Unicornuate Uterus
- A unicornuate uterus occurs when only one Mullerian duct develops properly, leading to a uterus that is smaller and shaped like a single horn. In some cases, a rudimentary horn (a small, underdeveloped uterine tissue) may also be present. Women with this condition may experience infertility, recurrent miscarriages, or an increased risk of ectopic pregnancies, as the single horn may not provide the proper environment for a growing fetus.
3. Uterus Didelphys
- This anomaly involves the complete failure of the two Mullerian ducts to fuse during fetal development, resulting in two separate uterine cavities, two cervixes, and sometimes a divided vagina. Although women with uterus didelphys can have successful pregnancies, they may face complications such as preterm labor, miscarriages, or difficulties during delivery due to the unusual uterine shape.
4. Bicornuate Uterus
- A bicornuate uterus is the result of partial fusion of the two Mullerian ducts, resulting in a uterus with two horns instead of one. This anomaly can lead to fertility issues, miscarriages, and complications during pregnancy, such as breech presentation or preterm labor.
5. Septate Uterus
- A septate uterus occurs when the two Mullerian ducts partially fuse but fail to completely merge, leaving a fibrous or muscular septum (a dividing wall) inside the uterus. This condition can cause infertility, repeated miscarriages, and complications with full-term pregnancies.
6. Arcuate Uterus
- An arcuate uterus is a mild abnormality in the fusion of the Mullerian ducts, resulting in a slightly indented uterine cavity. While this condition is generally less severe and may not cause fertility problems, it can still lead to complications such as preterm labor or a higher risk of miscarriage.
7. Diethylstilbestrol (DES)-Related Anomalies
- Although not a congenital Mullerian anomaly, exposure to the synthetic estrogen diethylstilbestrol (DES) during the early stages of pregnancy (typically between the 1940s and 1970s) is associated with developmental abnormalities in the reproductive organs of daughters born to women who used DES. These include structural abnormalities like a T-shaped uterus, which can cause infertility, miscarriage, or premature labor.
Symptoms of Mullerian Anomalies
The symptoms of Mullerian anomalies can vary depending on the specific condition and its severity. Some women may experience no symptoms at all, while others may encounter challenges related to fertility, menstruation, or pregnancy. Here are some common symptoms associated with Mullerian anomalies:
- Absent or Irregular Menstruation: Women with Mullerian anomalies like MRKH may not menstruate, or their menstrual cycles may be irregular.
- Painful Periods (Dysmenorrhea): Conditions like a septate or unicornuate uterus can cause painful periods, as the abnormal structure may lead to difficulty with menstrual blood flow.
- Infertility: Many Mullerian anomalies, especially those affecting the uterine structure, can lead to fertility issues due to the altered shape or size of the uterus or the presence of fibrous tissue.
- Miscarriages: Women with anomalies such as a septate uterus or a unicornuate uterus may experience recurrent miscarriages due to the inability of the uterus to properly support a growing fetus.
- Complications During Pregnancy: Women with a bicornuate uterus or uterus didelphys may face complications such as preterm labor, breech presentations, or a higher risk of cesarean deliveries.
Diagnosing Mullerian Anomalies
Mullerian anomalies are typically diagnosed through a combination of clinical evaluation, imaging studies, and sometimes surgery. Common diagnostic methods include:
- Ultrasound: A pelvic ultrasound can provide an initial assessment of the shape and size of the uterus and other reproductive organs.
- MRI (Magnetic Resonance Imaging): An MRI offers a more detailed and accurate picture of the uterus and surrounding organs, helping to identify structural abnormalities.
- Hysterosalpingography (HSG): An X-ray test that involves injecting a contrast dye into the uterus, which can reveal abnormalities like a septate or bicornuate uterus.
- Laparoscopy: In some cases, a minimally invasive surgical procedure may be required to directly view the internal reproductive organs and confirm a diagnosis.
Treatment Options for Mullerian Anomalies
Treatment for Mullerian anomalies largely depends on the type of anomaly, the severity of symptoms, and the individual’s reproductive goals. While some women may not require treatment, others may benefit from various interventions to improve fertility and pregnancy outcomes. Treatment options include:
1. Surgical Treatment
- Resection of a Septate Uterus: In cases of a septate uterus, surgery to remove the septum can improve fertility and decrease the risk of miscarriage. This procedure is often performed via hysteroscopy.
- Corrective Surgery for Unicornuate or Bicornuate Uterus: Surgery may be needed to correct the shape of the uterus, though this is typically reserved for cases where fertility is affected or the individual faces complications during pregnancy.
- Creation of a Vagina: For women with MRKH, surgical creation of a vaginal canal (vaginoplasty) may be recommended to improve sexual function.
2. Fertility Treatment
- Assisted Reproductive Technologies (ART): Women with Mullerian anomalies who experience infertility may benefit from ART, including in vitro fertilization (IVF), to achieve pregnancy.
- Surrogacy: In cases where the uterus is absent or unable to carry a pregnancy, surrogacy may be considered as an option for having a child.
3. Monitoring and Support During Pregnancy
- Women with Mullerian anomalies often require close monitoring during pregnancy, especially if they have a high-risk anomaly. Ultrasound examinations may be frequent to check for complications such as preterm labor or fetal growth restriction.
Conclusion
Mullerian anomalies are a diverse group of congenital conditions that can impact a woman’s reproductive health, but with appropriate diagnosis and treatment, many women with these anomalies can lead fulfilling lives and achieve their reproductive goals. If you suspect you may have a Mullerian anomaly, seeking guidance from a healthcare provider specializing in reproductive health is essential to understanding your options and receiving the support you need.